What to Expect
Discover helpful insights for the road ahead
Discover helpful insights for the road ahead For many patients and their families, receiving a diagnosis of Lambert-Eaton myasthenic syndrome (LEMS) is a great relief! After years of searching for an answer to their mysterious and debilitating symptoms, finally uncovering the cause of their muscle weakness and fatigue is a positive experience. For others, learning that they have a lifelong condition that may worsen over time causes fear and concern. If you or your loved one has just been diagnosed with LEMS, chances are, you’re feeling a little bit of both. Fortunately, knowledge is power, and diagnosis is usually a great jump-start for most patients.
Now that you know it’s LEMS, you can focus on learning what to expect and what you need to do. (Hey, you’re already doing that by visiting this website!) On this page, you’ll learn how LEMS can progress over time and how treatment can help. You’ll also find considerations for managing symptoms today and tomorrow.
HOW LEMS MAY PROGRESS
Although symptoms can vary from patient to patient, the first sign of LEMS is often muscle weakness in the legs and lower body. LEMS symptoms may progress and affect muscles in other areas as well as the part of the nervous system that controls basic bodily functions, leading to symptoms such as dry mouth, constipation, dizziness, and erectile dysfunction. Symptoms may progress more quickly in cases where cancer is involved.
Potential consequences of a delay in diagnosis or
treatment of LEMS
Spread and severity of symptoms
Loss of function and mobility
Loss of independence and quality of life
Everyday Habits That CAN MAKE A DIFFERENCE
As with any chronic condition, there are things that you can do to help maintain your health and daily activities. Be sure to check with your doctor before starting any new exercise regimen or trying a change in diet.
Stay on schedule
Be sure to follow your doctor’s prescription as closely as possible—particularly at the start of treatment, when your doctor may make dosage adjustments to provide you with the best relief of your symptoms.
Exercise moderately
With your doctor’s approval, consider light weight training or physical therapy to help improve stamina and maintain muscle strength. Daily walking and breathing exercises may also increase your energy levels.
Get enough sleep
A full night’s rest may help you manage fatigue and reduce stress. To make it easier to fall asleep, try to limit alcohol, caffeine, and screen time in the evening before going to bed.
Eat a healthy diet
A healthy diet can give your body the fuel it needs to stay energized and minimize fatigue.
MANAGING LEMS OVER TIME
Over time, LEMS symptoms may change or worsen, although that is hard to predict. In addition, as we age, we naturally lose muscle mass and function. Planning for long-term LEMS management can help you or your loved one stay active and maintain independence.
Keep a symptom journal
Check in with yourself regularly and record how you’re responding to treatment and any symptoms you may be noticing. Also, check in with your doctor regularly to see if a simple dose adjustment may provide even more relief.
To help you get started, download a free symptom tracking journal

Build an exercise plan
Ask your doctor, physiatrist, or physical therapist about tailoring an exercise plan for you that will help keep your bones and muscles strong, flexible, and functional now and in the future.
Some patients with neuromuscular conditions have found that hydrotherapy (exercise in a pool) is a low-impact way to strengthen muscles and relieve pain, stress, and fatigue.
Fall-proof your home
The last thing a LEMS patient needs is a slip and fall. Inspect your home for tripping hazards such as slippery floors, loose rugs, or cluttered walkways. Consider adding handrails to staircases, bathrooms, and showers for added stability. Your insurance company may pay for an occupational therapist to assess your home for safety and provide suggestions for making everyday activities easier.
Protect against health emergencies
A medical ID bracelet or pendant can provide identification if you’re ever in need of assistance and unconscious or unable to speak. Consider using a personal medical alarm help-button system such as LifeAlert® for further security and peace of mind for yourself or your loved one.
Make a long-term plan
Sit down with your family or caregiver and have an honest discussion about the future. Discuss your concerns, fears, and expectations, and then listen to theirs. Come up with a plan of support that you’re both comfortable with, and be sure to consider contingencies that may arise. Life is full of demands, and change is the only constant. Planning ahead now means that no one is left behind.
LOOKING FOR ADVICE?
The LEMS Aware blog is filled with insights from patients and caregivers. Get travel tips, learn about LEMS and exercise, and see how others are living their life with LEMS to the fullest!
CONSIDERATIONS FOR WHEN YOU’RE…
…SEEING THE DENTIST
- Schedule smart. Try to book your appointments for the morning or whenever your strength is at its best
- Keep your dentist informed. Let them know if you have trouble opening and closing your mouth, holding your head up, or swallowing
…HAVING SURGERY
- Consult your neurologist. Whenever possible, involve your neurologist in the planning of any surgery or procedure
- Time your procedure mindfully. Schedule your surgery for the morning, preferably as the first appointment of the day, when your muscle strength is at its best
- Avoid certain medications. Tell the healthcare team that you have LEMS and are extremely sensitive to neuromuscular blocking agents, which are often used during surgery for muscle relaxation
- Discuss anesthesia options. If you’re having a procedure on an external part of the body (like an arm, leg, or face), ask the healthcare team about using a local anesthetic. Tell them you have LEMS so they can avoid techniques that may impair your breathing
- Optimize your treatment. If possible, postpone any non-emergency surgery until your neurologist has optimized your treatment plan and adjusted or stopped any medications that could worsen your symptoms
…SEEING YOUR PRIMARY CARE DOCTOR
- Make an appointment plan to ensure that you get everything you need from the visit. Write down things that you want to discuss, including what has changed since the last visit, concerns about new symptoms or side effects, and any questions you may have
- Record the appointment using your phone or another device to ensure that you don’t miss any directions or details the physician gives you. (Be sure to get the doctor’s permission before recording)
- Update your treatment plan following the appointment. The plan should contain detailed information about your symptoms and current medications. If your doctor provides an after-visit summary, use that to help make updates
- Keep track of your medical records in 1 designated place so your information doesn’t get lost
…TRAVELING
- Discuss your travel plans with your doctor to make sure that the location and activities you have planned are safe or if you need to take any extra precautions
- Talk to your doctor about your medicines. Discuss your travel plans with your doctor to get guidance about how to safely carry your medications with you. For example, you may need a doctor’s authorization to carry your prescription medication through airport security. You can also get your prescription refilled at your destination
- If you have trouble walking, check with the airport or train station if you think you may need to travel with medical equipment such as a walker, a wheelchair, or an electric scooter
- Carry important paperwork on your person, not in your checked luggage. You don’t want to lose important documents like your health insurance card, travel insurance, or your physician’s letter detailing any medical equipment or medication needed during travel
- If you feel unwell during travel, alert the flight attendant, train conductor, or other personnel immediately before the situation worsens
- Be prepared to deal with the climate and environment at your destination. Make sure to pack the right clothes to keep yourself warm or cool and items like sunscreen and sunglasses, if appropriate
- If you’re planning travel to a warmer climate, keep in mind that getting overheated can make LEMS symptoms worse. Make sure to stay hydrated, avoid prolonged periods in the sun, and take cool showers
- Know the location of local clinics for timely medical care or access to wheelchairs or motorized scooters. You may not use them at home, but travel can be taxing, and being in a different place may require that you receive a little more help getting around
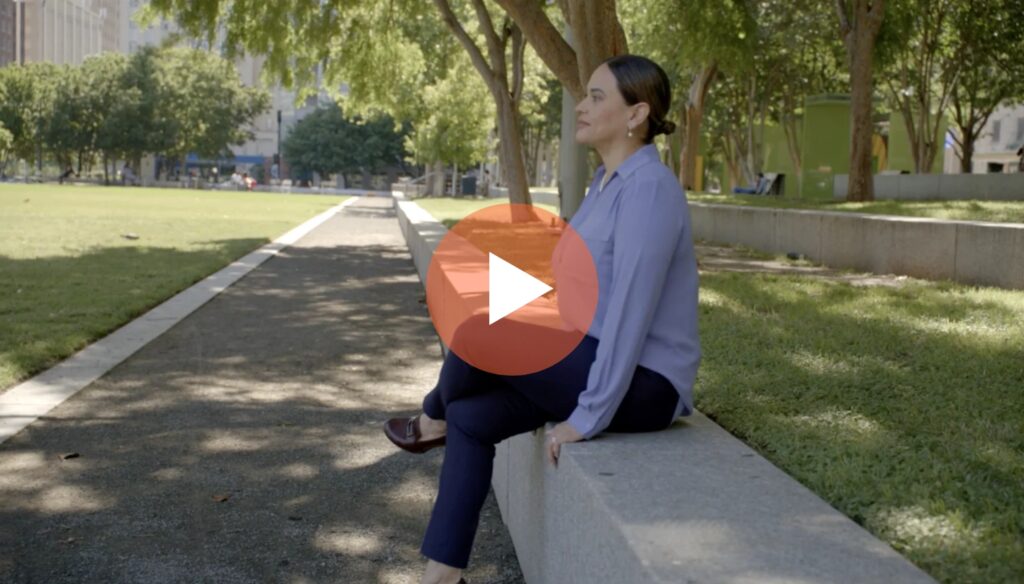
And I know that I’ve been given this disease because I can handle it, and I need to serve.
Advocating for yourself and others
Desiree talks about leveraging her background as a nurse to educate other patients and healthcare providers about LEMS, the importance of an early diagnosis, and the need for the rare disease community to advocate for themselves.